Dr. Audrey Talley-Rostov on Increasing Awareness for Keratoconus
Have you recently noticed any changes in your vision? For many this can signal changes in your eye health, such as the development of astigmatism, but for others, an unexpected change can indicate a more serious problem. Keratoconus, a progressive eye condition in which the cornea weakens and thins over time causing the development of a cone-like bulge, is one of these conditions.
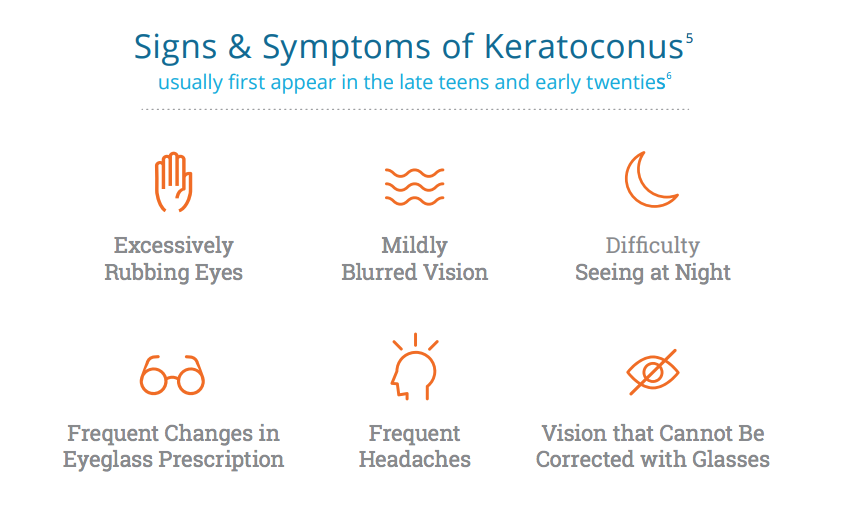
While symptoms for keratoconus often first appear in the late teens and early twenties, there are instances where a diagnosis may come later in life. Keratoconus can often be misdiagnosed, as symptoms can be confused for other more common conditions. If left untreated, it can result in significant visual loss.
With new diagnostic tools allowing for earlier diagnosis and an increase in awareness of the condition among people and physicians, keratoconus is being detected sooner and more accurately. It’s important to call the eye doctor if you notice changes in your or your family’s vision.
We recently spoke with Dr. Audrey Talley-Rostov of Northwest Eye Surgeons about when someone should be screened for keratoconus, the importance of early diagnosis, and how keratoconus awareness has developed over the years.
How do you determine if someone should be screened for keratoconus? What are the warning signs?
Anyone who has increasing astigmatism, a family history of keratoconus and/or significant change in vision, especially in childhood or teenage years, should be screened for keratoconus. However, adults over 40 can also have changes and development or progression of this condition. It is important to be aware of increasing astigmatism, as this may be the first sign of keratoconus.

Why are awareness and early keratoconus diagnosis important for someone’s short and long-term eye health?
Early diagnosis of keratoconus can prevent the progression of this condition and the need for corneal transplantation1. In addition, other behavior factors, such as eye rubbing, can be recognized and modified. Dry eye, which can accompany keratoconus, can also be diagnosed and treated appropriately, potentially decreasing eye rubbing behavior, and improving overall eye health.
How has awareness for keratoconus changed in the last five years?
I am encouraged that more eye care practitioners are becoming aware of keratoconus and therefore screening patients or referring patients for screening if they do not have the diagnostic equipment themselves. Topography and tomography systems are extremely helpful for screening potential keratoconus patients. There are now software applications that are included in some of these devices that are helpful for early detection and progression of the condition.
To find a doctor near you to get screened for keratoconus, use our locator tool.
For more information on keratoconus or to hear people’s personal experiences with the condition, visit our website and follow us on Twitter, Facebook, and Instagram.
Dr. Rostov is a paid consultant of Glaukos.