What To Know About Corneal Topography – Part 1
Whether you’ve worn glasses or contacts for years or not, realizing your vision is declining can be a scary experience. For patients suspected to have keratoconus, an eye condition that causes progressive thinning and bulging of the cornea, doctors may order multiple tests to view your cornea and determine the root cause of your symptoms, with corneal topography as one popular diagnostic tool.
However, many people who first hear the term corneal topography don’t know what it is, why it’s important, or what to expect.
This is Part 1 of a two-part blog series, which will be released over the following weeks.
How is keratoconus diagnosed?
In many cases, the first signs that a patient may have keratoconus include:
- Frequent changes in eyeglass prescription
- Vision that cannot be made clear even with new eyeglasses
- Family histories of keratoconus
- Frequent eye rubbing
During an exam to diagnose whether a patient has keratoconus, his or her corneas are examined using a slit lamp microscope, to look for areas that are thin, steep, or show other findings associated with keratoconus.
The thickness of the central cornea may be measured using a device called an ultrasound pachymeter and compared to the thickness measured in other parts of the cornea, to look for areas that show signs of thinning.
The shape of the cornea is imaged using a corneal topographer or tomographer, and the images obtained are analyzed to look for areas that appear abnormally steep or irregularly shaped. Changes in corneal curvature provide information about whether the condition shows signs of progression (worsening).
What is corneal topography and why would my doctor recommend this?
Corneal topography is an imaging technique that is used to create a color-coded map of the curvature of the cornea using a specialized camera and computerized analysis. This information allows your doctor to assess whether there are any abnormalities in corneal shape that may indicate keratoconus or other disorders. Additionally, corneal topography can provide information that is useful in fitting a contact lens to the unique shape of the cornea.
While keratoconus can sometimes be diagnosed with a single visit, repeated corneal topography may be obtained at follow-up visits to determine whether the cornea is becoming steeper or more irregular over time. Changes in corneal curvature may indicate progression of keratoconus.
What is the difference between corneal topography and tomography?
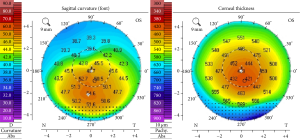
Corneal topography provides a map of the front surface of the cornea that is used to evaluate its curvature.
Corneal tomography also provides a map of the front surface, as well as additional information about the curvature of the back surface of the cornea (inside of the eye). Corneal tomography may also be used to create a map showing the thickness of different areas of the cornea.
Both corneal topography and corneal tomography can be useful in the diagnosis of keratoconus.
Is there anything that I need to do before having a corneal topography exam?
Generally, there is nothing special you need to do before having a corneal topography exam. If you wear contact lenses, you will need to remove them for the corneal topography exam.
In certain situations, your doctor may ask you to remove your contact lenses for a few days or even weeks before undergoing corneal topography in order to improve the accuracy of the measurement or to rule out any temporary changes to corneal shape caused by contact lens wear. It is always a good idea to check with your doctor regarding whether you should come into the office for your appointment while wearing your contact lenses.
Learn more: What You Need To Know About Corneal Topography – Part 2
To find a doctor near you to get screened for keratoconus, use our locator tool.